FALL 2021, THE EVIDENCE FORUM, WHITE PAPER
 David January, PhD, MWC Associate Scientific Director Evidence Synthesis, Modeling & Communication Evidera, a PPD business |
Introduction to NGS
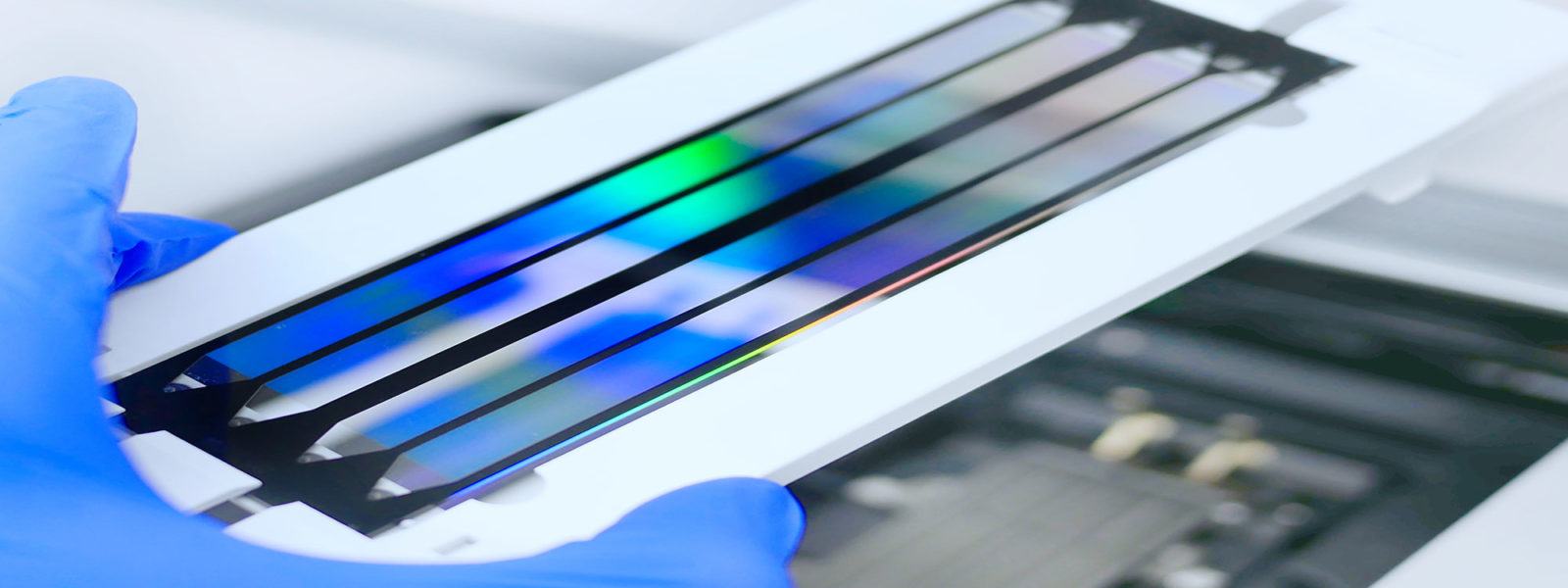
The term “next-generation sequencing” (NGS) refers to a variety of technologies that allow for rapid, high-throughput genetic sequencing.1,2 NGS technologies allow for much faster, less expensive sequencing of the genes in a sample than the conventional Sanger sequencing technique, which is restricted to sequencing specific genes one at a time.1,3 NGS also allows for the identification of multiple allelic variants (alternate forms of the same gene) simultaneously, whereas only one allelic variant can be identified per sequencing run when using older sequencing methods.1 NGS technologies achieve this increase in speed and identification of allelic variants by fragmenting DNA into shorter strands of base pairs and performing the sequencing reaction for each fragment simultaneously.2
The decreased cost and potential for rapid whole genome sequencing afforded by NGS technologies has many potential applications in healthcare. One area of use is in newborn screening for genetic diseases.4-6 NGS has been widely used to determine whether newborns have genetic variants associated with lysosomal storage disorders and other inborn errors of metabolism, allowing for potentially earlier diagnosis and treatment to avoid the progressive clinical deterioration, disability, and, ultimately, mortality resulting from these diseases if left untreated.5 NGS can also be used to diagnose genetic diseases after patients present with clinical manifestations, and the ability to target multiple allelic variants simultaneously may help reduce the sometimes long and difficult diagnostic journey for patients who present with symptoms associated with several differential diagnoses.2,5
Another area of focus for the use of NGS technologies has been oncology. NGS can be used to test for germ-line mutations to establish a patient’s risk for developing certain cancers, such as with the BRCA mutation.7 NGS can also be used in a complementary fashion to assess cancerous tissue directly for certain genetic mutations that might predict response to certain anti-cancer agents, such as for del(17p) chronic lymphocytic leukemia (CLL).2,8,9 This latter use is the focus of this paper. As of 2017, most oncologists in the United States (US) reported relying on NGS tests when making decisions relating to treatment for their patients.10 Further, several of the newer oncology therapeutics being released are very targeted for specific mutations and do not work well for tumors with different genotypes (for example, Herceptin’s indication in HER2 overexpressing tumors or tumors with HER2 gene amplification).11 Foundation Medicine maintains a list of over 20 such therapies at their website: https://www.foundationmedicine.com/test/foundationone-cdx. As these newer, powerful, targeted treatments are typically very expensive,12 NGS may be useful in identifying those patients who are most likely to benefit from the treatments and avoid inefficient healthcare spending. This recognition of the usefulness of NGS in guiding treatment decisions for patients with cancer, and the potential to make use of these targeted therapies economically feasible, highlight the urgency of the question of how these tests can gain reimbursement and wider use. This paper explores this question.
Download White Paper
Fill out the form below to download this whitepaper.