SPRING 2019, THE EVIDENCE FORUM, WHITE PAPER
 Kevin Marsh, PhD Executive Director Commercial Strategy andNew Product Development Patient-Centered Research, Evidera |  Margaret Vernon, PhD Vice President and General Manager Patient-Centered Research, Evidera |
Introduction
The last 10 years have seen the complexity of clinical trials increase – the number of procedures involved in trials has increased by 59% and planned visits have increased by 25%.1,2 This complexity has coincided with declining numbers of patients who are eligible and recruited per site, increasing the need for a larger number of investigative sites and countries in which drug makers are conducting trials.2 In that context, it is perhaps unsurprising that a third of trials fail to meet their recruitment targets, and more than half of trials need to be extended to do so.3 Trials are correspondingly either underpowered or more costly and time intensive to conduct.
These issues are compounded in rare disease populations where recruitment difficulties can arise for several reasons, including:
- Small populations distributed over wide geographic areas
- Many rare diseases being paediatric
- Patients often being highly frail
- There being few centers for diagnosis
- A scarcity of investigators focused on these rare diseases4
Furthermore, there is often little, if any, experience of conducting studies with rare disease populations, meaning a lack of knowledge about which trial designs work for these special populations. To conduct a successful trial program, it is imperative that trials are designed and implemented in such a way as to enhance patients’ and caregivers’ experiences and reduce burden and complexity. This is likely to be particularly true in a rare disease population, which may require some special accommodation in order to participate in the trial and can be facilitated by engaging patients in the design of trials. Patient engagement has become a hot topic in recent years, and many high-profile initiatives have advocated for and facilitated patient engagement in research and decision making throughout the drug development process.5-8 In January 2019, the US Food and Drug Administration (FDA) published its draft guidance on rare diseases, Rare Diseases: Common Issues in Drug Development Guidance for Industry, which includes a section on the importance of patient and caregiver engagement in rare disease clinical trials to ensure patients’ and caregivers’ perspectives about experiences, expected and desired outcomes of treatment, and needs are taken into account.9
To conduct a successful trial program, it is imperative that trials are designed and implemented in such a way as to enhance patients’ and caregivers’ experiences and reduce burden and complexity.
Key stakeholders have acknowledged the important role that patients can play in the design of clinical trials for treatments for rare diseases. For instance, the National Institutes of Health (NIH) Office for Rare Disease Research (ORDR) established the Rare Disease Clinical Research Network (RDCRN). The RDCRN was unique in being the first program that created a collaborative and coordinated network of investigators and patient groups to support research into rare diseases. The network comprises 22 research consortia, of which 82% report patient groups reviewing protocols and providing substantial input on study design, and 94% report patient groups reviewing study forms and other study related documents.4
More recently other rare disease organisations have encouraged the involvement of patients in the design of clinical trials in rare diseases. EURORDIS-Rare Diseases Europe has published a charter for the collaboration between study sponsors and patient organisations, with the aim of improving the quality of clinical research in rare diseases,10 and Genetic Alliance has published a guide for sponsors and investigators on involving patients in clinical research.11
How can patients be engaged in trial design and implementation?
Engaging patients in trial design and implementation plans can help ensure:
- The patients included in trials are those that are likely to have a positive benefit-risk balance
- The endpoints included in the trial capture experiences and outcomes of treatment most important to patients
- The trial is conducted in such a way as to enhance experience and ease burden
We specifically focus this paper on the experience of and burden on the patient participating in the trial.
Patients can be instrumental in providing input on designs and operational implementation of trials that enhance enrollment and retention. Patient input on protocol design can identify potential barriers to participation and retention and support development of appropriate solutions, such as:
- Modifying design elements of the trial to ensure that patients think there is value in the study objective
- Development of key messages and outreach materials to enhance enrollment
- Development of logistical support, such as transportation, in the case of obstacles such as format, location, scheduling, length, and timing of assessments
- Engagement and retention strategies – such as providing patient-friendly communications, gamification, or incentives – in the case of a trial design that has been identified as lengthy or potentially burdensome
- Tailoring solutions to ensure the feasibility of trial participation in specific populations, perhaps identified by geographic location
Figure 1 summarizes methods that have been adopted to elicit patients’ input into protocol design. Involving patients as partners ensures that their views are available as part of the research team, which is insightful in itself but can also enhance implementation of other engagement activities. One-on-one interviews and focus groups can provide an in-depth characterization of the patient experience and perception of trial designs. Simulations, such as mock trial visits, may help patients and other stakeholders understand what is involved in a trial and allow them to comment on the relative burden or potential barriers to participation or adherence with trial procedures. Quantitative methods, such as surveys embedded in trials, can characterize the clinical trial experience for a broader set of patients and help to inform trial interpretation or future trial designs. Crowd sourcing can offer feedback on elements of the protocol from a larger, more diverse sample. Finally, preference methods can be used to understand the burden that trials place on patients. For instance, running choice experiments with patients – giving them pairs of trials each characterized by different time and travel commitments, and involving different numbers and types of assessments – allows us to understand how changing the design of a trial will impact the probability that a patient will participate, and how this varies between different groups of patients.
Figure 1. Methods for Eliciting Patient Input into Protocol Design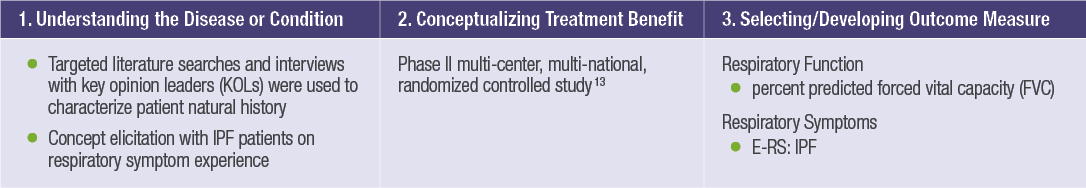
What are the benefits of involving patients in trial design and implementation planning?
As a relatively new practice, there is limited public evidence on the time and cost savings of gathering patient input on protocol design, particularly in rare diseases. A recent review of patient involvement in the rare disease product development process concluded that, to date, patient opportunities for involvement in clinical trials have solely comprised enrollment as trial subjects,12 and involvement in the design of trial has been confined to patient organizations (for instance, see those mentioned in the introduction).
Nevertheless, the evidence that does exist is encouraging. First, a recent review published in the BMJ identified26 studies on the impact of patient or public engagement on study enrollment and retention.13 Nineteen of the studies were eligible for a meta-analysis of enrollment rates, and five for a meta-analysis of retention rates. The review concluded that patient and public engagement in study design increases the odds of participant enrollment. No impact was identified on retention rates, due to the smaller sample of studies addressing retention rates, and the nature of interventions varying between studies.
Second, the expected net present value (ENPV) of patient engagement in a typical oncology development program entering Phase II or Phase III has been modeled.14 Assuming that a protocol review with a patient group results in the avoidance of one amendment, the authors estimate patient engagement increases the ENPV at pre-Phase III by $75 million. Put another way, a $100,000 patient engagement exercise would only have to reduce the probability of needing an amendment by approximately 0.1% before it justified its cost. That is, the costs of gathering patient input on protocol design are relatively low compared to the potential benefits: every time a patient drops out of a study, it can cost up to $36,000 to add a new patient, sometimes requiring the opening of new sites depending on dropout rates.15
Finally, analyses of trial databases, such as Trialtrove® and Pharmaprojects®, suggest that drugs developed with patient-centric designs are:
- Quicker to recruit 100 patients (4 months) than drugs developed without such designs (7 months)
- More likely to be launched (87%) than drugs developed without such designs (68%)16
Conclusion
In summary, involving rare disease patients and their caregivers in drug development, and particularly protocol design and operational implementation planning, could provide myriad benefits to the trial sponsor and the target patient and caregiver community at large. Benefits for sponsors include faster enrollment and reduced drop out, including associated costs. Perhaps the greatest benefit is for the patients, including reducing the hurdles to participating in trials, reducing unnecessary burden and complexity for patients participating in trials, and getting drugs to market faster for patients who need them the most.
References
- Getz KA, Campo RA. New Benchmarks Characterizing Growth in Protocol Design Complexity. Ther Innov Regul Sci. 2018 Jan;52(1):22-28. doi.org/10.1177/2168479017713039. Epub 2017 Jun 23.
- Tufts CSDD (Center for the Study of Drug Development) Impact Reports. Rising Protocol Complexity is Hindering Study Performance, Cost, and Efficiency. July/August 2018;20(4). Available at: https://csdd.tufts.edu/impact-reports/. Accessed February 20, 2019.
- Treweek S, Lockhart P, Pitkethly M, et al. Methods to Improve Recruitment to Randomised Controlled Trials: Cochrane Systematic Review and Meta-Analysis. BMJ Open. 2013 Feb 7;3(2). pii:e002360. doi:10.1136/bmjopen-2012-002360.
- Merkel PA, Manion M, Gopal-Srivastava R, et al. and for the Rare Diseases Clinical Research Network. The Partnership of Patient Advocacy Groups and Clinical Investigators in the Rare Diseases Clinical Research Network. Orphanet J Rare Dis. 2016 May 18;11(1):66. doi: 10.1186/s13023-016-0445-8.
- Patient-Centered Outcomes Research Institute (PCORI). National Priorities for Research and Research Agenda. May 21, 2012. Available at: https://www.pcori.org/assets/PCORI-National-Priorities-and-Research-Agenda-2012-05-21-FINAL.pdf. Accessed February 20, 2019.
- US Food and Drug Administration. The Voice of the Patient: A Series of Reports from FDA’s Patient-Focused Drug Development Initiative. Available at: https://www.fda.gov/forindustry/userfees/prescriptiondruguserfee/ucm368342.htm. Accessed February 20, 2019.
- European Patients’ Academy (EUPATI). Available at: https://www.eupati.eu/. Accessed February 20, 2019.
- Congress.Gov. H.R.34 – 21st Century Cures Act, 114th Congress (2015-2016). Available at: https://www.congress.gov/bill/114th-congress/house-bill/34/. Accessed February 20, 2019.
- US Food and Drug Administration. Rare Diseases: Common Issues in Drug Development Guidance for Industry, Draft Guidance. Available at: https://www.fda.gov/ucm/groups/fdagov-public/@fdagov-drugs-gen/documents/document/ucm629579.pdf. Accessed February 20, 2019.
- EURORDIS-Rare Diseases Europe. Charter for Clinical Trials in Rare Diseases – EURORDIS Charter for Collaboration between Sponsors and Patient Organisations for Clinical Trials in Rare Diseases. Available at: http://www.eurordis.org/IMG/pdf/Charter_Clinical_Trials-Final.pdf. Accessed February 17, 2019.
- PatientPartner Project, funded by the Framework Programme of the European Commission. Patient Involvement in Clinical Research: A Guide for Sponsors and Investigators. Available at: https://www.geneticalliance.org.uk/media/1603/patientpartnersponsor.pdf. Accessed February 19, 2019.
- Young A, Menon D, Street J, Al-Hertani W, Stafinski T. Exploring Patient and Family Involvement in the Lifecycle of an Orphan Drug: A Scoping Review. Orphanet J Rare Dis. 2017 Dec 22;12(1):188. doi: 10.1186/s13023-017-0738-6.
- Crocker JC, Ricci-Cabello I, Parker A, et al. Impact of Patient and Public Involvement on Enrolment and Retention in Clinical Trials: Systematic Review and Meta-Analysis. BMJ. 2018 Nov 28;363:k4738. doi: 10.1136/bmj.k4738.
- Levitan B, Getz K, Eisenstein EL, et al. Assessing the Financial Value of Patient Engagement: A Quantitative Approach from CTTI’s Patient Groups and Clinical Trials Project. Ther Innov Regul Sci. 2018 Mar;52(2):220-229. doi: 10.1177/2168479017716715. Epub 2017 Jul 17.
- Pharmaceutical Research and Manufacturers of America (PhRMA) and Battelle Technology Partnership Practice. Biopharmaceutical Industry-Sponsored Clinical Trials: Impact on State Economies. March 2015. Available at: http://phrma-docs.phrma.org/sites/default/files/pdf/biopharmaceutical-industry-sponsored-clinical-trials-impact-on-state-economies.pdf. Accessed February 20, 2019.
- The Economist. The Innovation Imperative: The Future of Drug Development. Available at: https://druginnovation.eiu.com/. Accessed February 21, 2019.
For more information, please contact
[email protected] or [email protected]