FALL 2020, THE EVIDENCE FORUM, WHITE PAPER
 Meg Richards, PhD, MPH Senior Research Leader Real-World Evidence Evidera, a PPD business |  Ronna L. Chan, PhD, MPH Senior Research Associate Real-World Evidence Evidera, a PPD business |  Laura Sayegh, MScA Research Associate Real-World Evidence Evidera, a PPD business |
The COVID-19 pandemic has taught us much about the novel virus, and one of the more remarkable lessons is the variation in symptom presentation. Aside from the expected cough, muscle aches, and fever,1 there have been reports of “COVID tummy” (nausea, vomiting, diarrhea), “COVID taste loss,” and “COVID toes” (painful red lesions on the feet).2 Symptoms vary with age, general health status, and severity of COVID-19 infection, but according to some very recent research, the core symptoms present in a consistent order. University of Southern California (USC) researchers examined rates of symptom incidence collected by the World Health Organization (WHO) for over 55,000 confirmed COVID-19 cases in China. They modeled a sequence that begins with fever, moves to cough and muscle pain, then on to nausea, vomiting, and diarrhea.3 It’s a “head-to-toe” or “North-South” progression, more or less.
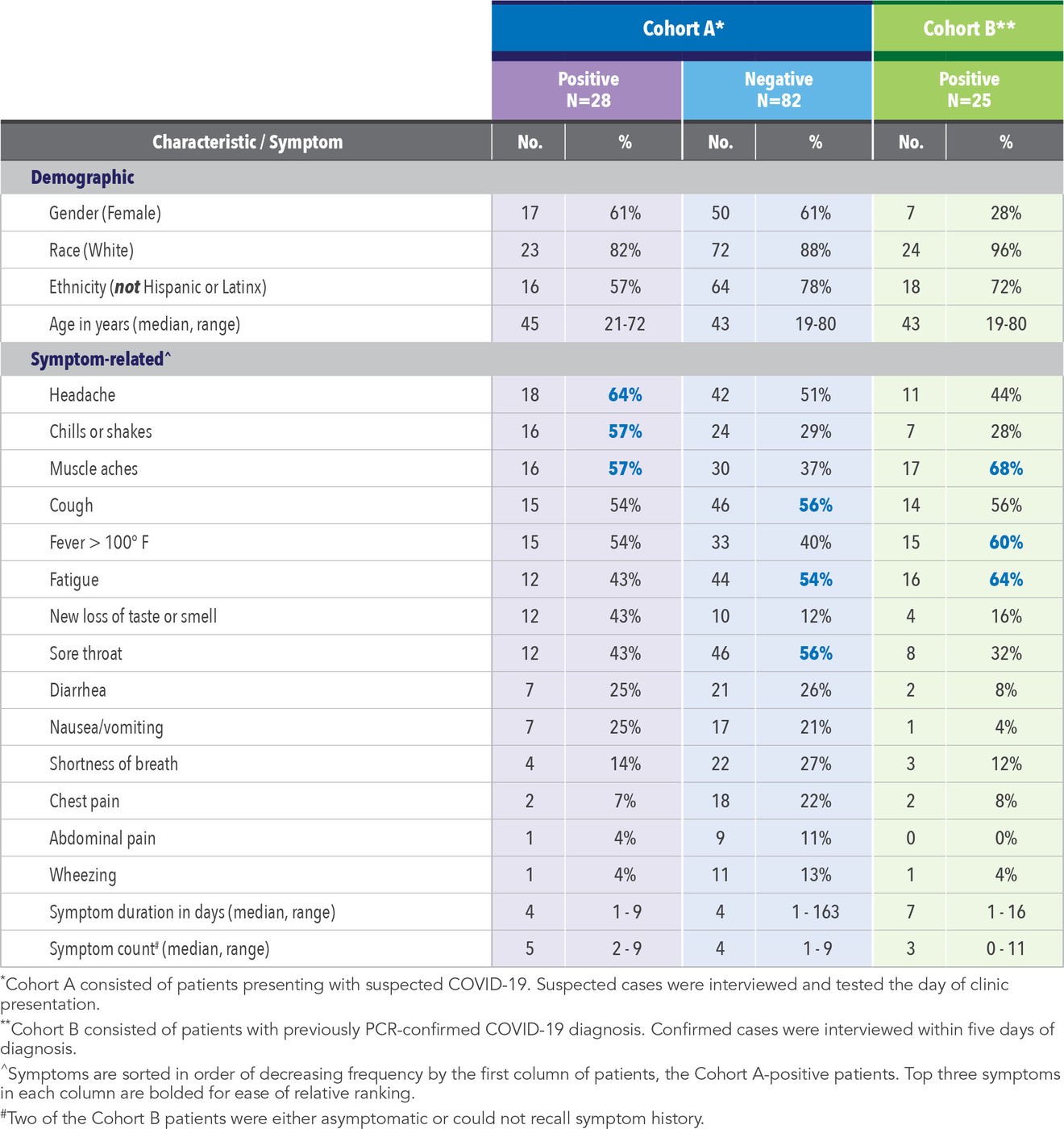
Evidera has had the opportunity to support a number of COVID-19 research projects, one recently completed. The study included two cohorts of patients at several primary care clinics in early summer of 2020 in the southwest United States (US). Cohort A consisted of patients presenting with suspected COVID-19, whereas Cohort B consisted of patients with previously polymerase chain reaction (PCR)-confirmed COVID-19 diagnosis. The suspected cases were interviewed and tested the day of presentation whereas the confirmed cases were interviewed within five days of diagnosis. Study participants were presented with a core symptom checklist and were asked to recall the day of symptom onset. Although they were not asked about symptom order, we hypothesized that because all patients were newly symptomatic, they would report more fever, cough, and muscle aches than later onset gastrointestinal symptoms. We were curious if the Cohort A patients who ultimately tested negative had a different profile than the Cohort A patients who ultimately tested positive, and how their profile might differ from Cohort B patients. The results are summarized in Table 1.
Of the 110 patients in Cohort A presenting with suspected COVID-19, 28 (25%) tested positive. Positive patients were more ethnically diverse than those testing negative (43% versus 22% Hispanic or Latinx) and were in a narrower age range (21-72 years versus 19-80 years). The most frequently reported symptoms for Cohort A-positive patients were headache, chills, and muscle aches, whereas for Cohort A-negative patients, cough, sore throat, and fatigue were the most common complaints. Number of symptoms and symptom duration were similar between the Cohort A-positive and -negative subgroups, with the exception of one reported (verified) symptom duration of 163 days for a patient who ultimately tested negative.
The most interesting contrast, perhaps, is between the Cohort A-positive patients and the Cohort B (positive) patients. Although Cohort A-positive patients were predominantly female (61%), Cohort B patients were predominantly male (28% female). Cohort A-positive patients were more racially diverse than Cohort B (82% versus 96% White, respectively). The most commonly reported symptoms for Cohort B included muscle aches, fatigue, and fever. Although Cohort A-positive patients reported a larger number of symptoms than Cohort B (a median of five versus three, respectively), reported duration of symptoms among Cohort A-positives was shorter than Cohort B (a median of four versus seven days, respectively.) It is likely that the Cohort B patients were more distant from symptom onset and diagnosis such that a longer reported duration of symptoms (and some recall bias) would not be unexpected.
Looking across the positives, it appears that the earlier symptoms in the USC-proposed progression – fever, cough, muscle pain – are indeed more prominent in these newly diagnosed/recently diagnosed COVID-19 patients than the later symptoms involving the GI tract. This holds true even for the Cohort A-negatives. It is interesting that sore throat – a rather nonspecific symptom of respiratory illness – is prominent among the negatives. Perhaps those who ultimately tested negative were actually suffering with rhinovirus or allergies. There are anecdotal reports of persons wishing to be tested for COVID-19 infection who manufacture symptoms in order to secure a test where tests remain in scarce supply.
Our interpretation of these data is limited by several factors. First, this is a cross-sectional convenience sample of patients from two study sites and with two sets of entry criteria (known to be COVID-19 positive versus presenting for COVID-19 work-up.) Patients who chose to participate may be quite distinct from those who were approached for participation but refused (we did not have the resources to collect information on refusals). Furthermore, we did not collect information on order of symptoms, severity of symptoms, or impact of illness on patients’ lives; these would be interesting endpoints to examine in future studies.
COVID-19 continues to teach, or as some have said, “to school,” us.4 Virologists submit that instead of using language that suggests “waging war” against the coronavirus, we embrace the notion that COVID-19 is tutoring us. Undoubtedly, the lessons we learn will continue well into 2021 and beyond.
References
- Centers for Disease Control (CDC). Symptoms of Coronavirus (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/downloads/COVID19-symptoms-11×17-en.pdf. Accessed September 9, 2020.
- Parker-Pope T. The Many Symptoms of COVID-19. The New York Times. Available at: https://www.nytimes.com/2020/08/05/well/live/coronavirus-covid-symptoms.html. Accessed September 9, 2020.
- Larsen JR, Martin MR, Martin JD, Kuhn P, Hicks JB. Modeling the Onset of Symptoms of COVID-19. Front Public Health. 2020 Aug 13; 8:473. doi: 10.3389/fpubh.2020/00473.
- Griggs MB. COVID-19 Just Schooled a Bunch of Universities. The Verge. Available at: https://www.theverge.com/2020/8/22/21396061/covid-19-antivirus-college-closingsantibodies-long-haul. Accessed September 9, 2020.
For more information, please contact
[email protected], [email protected], or [email protected].